You can come across different forms of pneumonia in your lifetime. There is not one specific type of pneumonia, but categorically three depending upon the type of pathogen. The basic three contagions are because of viral, bacterial, and fungal attacks on your immune system. Among the bacterial strains responsible for causing pneumonia, Streptococcus pneumoniae is the most common one.
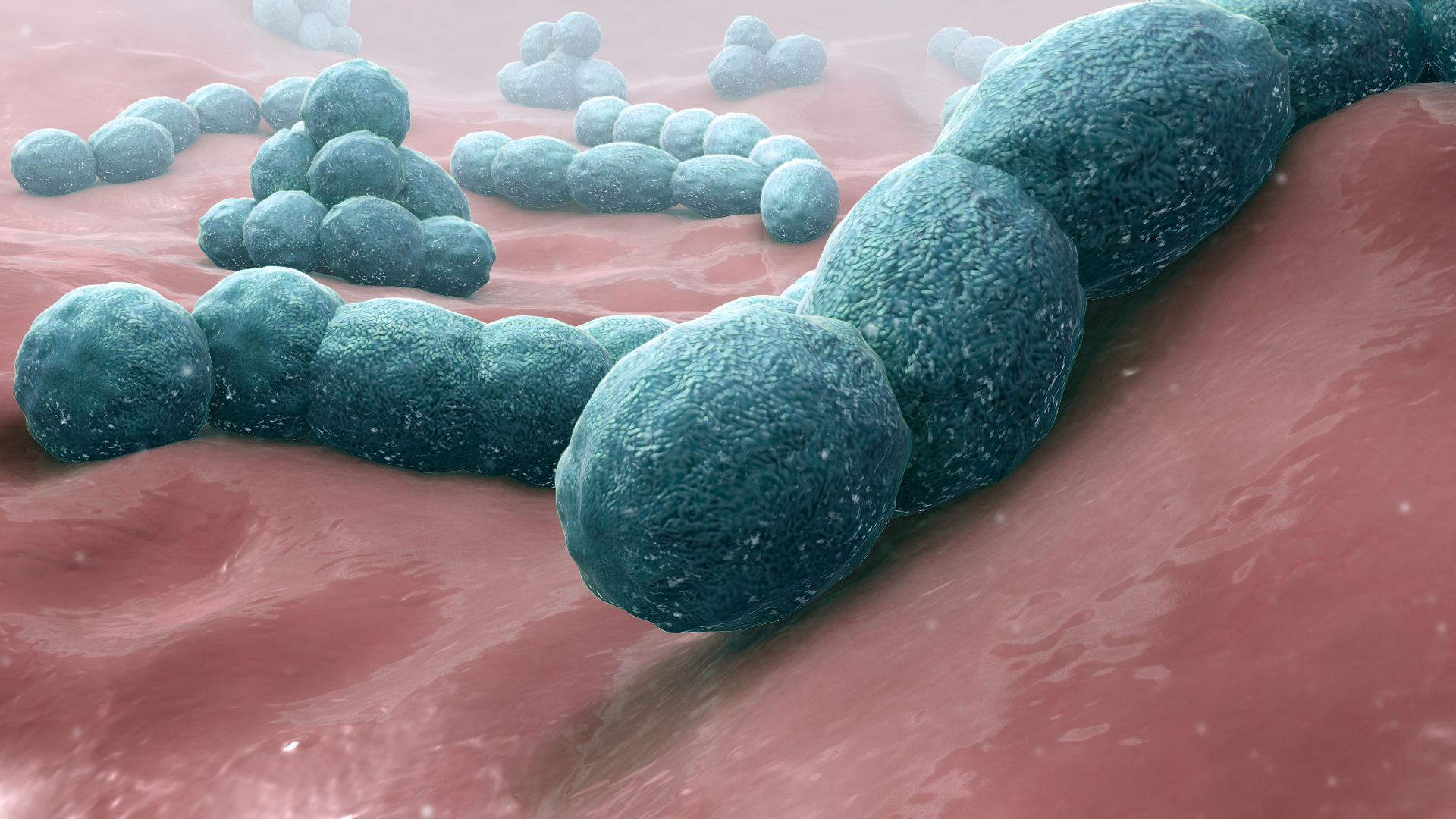
Streptococcus pneumoniae quite obviously belongs to the domain of bacteria, and phylum of Firmicutes. The class of Streptococcus pneumoniae is Bacilli, which specifies that it is a Gram-positive species. Order and family of the bacterium are Lactobacillales and Streptococcaceae respectively. Louis Pasteur (French chemist) and George Sternberg (physician) were the first to isolate Streptococcus pneumoniae concurrently, yet independently in 1881.
Later in 1886, Streptococcus pneumoniae became popular by the name of pneumococcus because of its causative role in pneumonia infection. Since 1920, the name of the bacterium changed to Diplococcus pneumoniae (existing in pairs). The change of name was mostly because of the way the organism appeared in sputum, on staining with Gram stain.
Again in 1974, the term Streptococcus pneumoniae was back in the medical field due to its similarity with streptococci. In an aerobic atmosphere, Streptococcus pneumoniae is alpha hemolytic in nature but beta-hemolytic in an anaerobic environment. Therefore, you can call Streptococcus pneumoniae as a facultative anaerobe belonging to the genus of Streptococcus.
Table of Contents
How is the infective rate of Streptococcus pneumoniae?
Streptococcus pneumoniae lacks the ability to form spores, and do not show any motility. For the first time in the nineteenth century, Streptococcus pneumoniae came into limelight due to several antibody-mediated immunity studies. It was then when scientists discovered that Streptococcus pneumoniae was root cause behind the pneumonia infection.
The bacterium usually exists in healthy individuals asymptomatically, forming colonies in the nasal cavity, sinuses and respiratory tract. If you have low level of immunity, you are more susceptible to infections like pneumonia. Therefore, infants and elderly population is at a greater risk of pneumonia infection due to their poorly developed immune system.
Streptococcus pneumonia can spread infections directly from infected persons to healthy ones on physical contact, or exposure to respiratory droplets. Pneumonia can prove to be a major neonatal disease.
How to differentiate Streptococcus pneumoniae from other streptococci?
Viridans streptococci is a big set of symbiotic streptococcal bacteria that are Gram-positive and alpha-hemolytic in nature. You can well distinguish Streptococcus pneumoniae from other streptococci using an optochin test, to which it is extremely sensitive. The strain is also sensitive to lysis on contact with bile, done using the bile solubility test.
The capsid or polysaccharide (protein coat) on the bacterium’s body is the actual virulence factor for Streptococcus pneumoniae. There are beyond 90 significant known serotypes of Streptococcus pneumoniae, which vary in prevalence, degree of drug tolerance and virulence.
What are the existing facts about pneumonia?
Pneumonia is a distinct pulmonary infection that you can well identify by the inflammation of alveolar sacs present within lungs. When fluid accumulation occurs in the air sacs due to pneumococcus invasion, you suffer from pneumonia. There are very less chances of you getting fungal pneumonia. You will mostly come across pneumonia from bacterial and viral strains.
Possible symptoms of pneumonia
When Streptococcus pneumoniae affects your immune system and alters its functioning, you come across the following signs:
- Sudden chills
- Constant coughs with mucus or pus that appear greenish or yellowish (sometimes blood as well)
- Fever going as high as 105°F
- Diarrhea
- Excessive sweating
- Feeling short of breath
- Fingernails and lips becoming bluish in color
- Experiencing pain in your chest during coughs
- Heart rate and breathing pace increases
- Losing your appetite very quickly
- Extreme fatigue
- Nausea accompanied with puking and headache
The symptoms will vary depending on your lifestyle and health status, as well as to which age group you belong. In case of newborns and children, the symptoms might not be that specific as in the case of adults.
If your child has pneumonia, you will mostly notice the unusual weariness and restless behavior. There can be signs of headache and vomiting as well, along with high fever.
The immunity level in older individuals gradually go down with age, thus increasing the possibility of infections including pneumonia. You will majorly find symptoms related with mental health, like a state of confusion in elderly people.
When should you be alert about pneumonia?
The period of incubation for pneumococcal infections mostly rely on the form of pathogen that is causing the disease. The incubation time of viruses, fungi, and bacteria is significantly different from one another.
Apart from the kind of contaminant, there are other factors as well that determine the maturation period of the microbe. Factors like biological state of the individual (immunological functioning), general health and age play a key role in pneumonia.
You will start noticing symptoms of pneumonia approximately ten days from the day of infection. The signs are quite similar to those of flu or common cold, but pneumonia signs take longer to show up.
How to distinguish between flu and pneumonia symptoms?
When you are having signs of runny nose, coughing or wheezing, you may often mix up flu and pneumonia. The early symptoms of both the infections are very alike, but have fine lines of difference.
Pneumonia is a typical infection of your lungs that mostly result in respiratory problems. However, flu is more of distinguishable by aches in the muscles along with fatigue. You can get flu only from viral strains, but pneumonia can happen due to bacteria, viruses as well as fungi.
The symptoms of flu are noticeable very quickly, taking from the onset of the infection. Possible signs include-
- Soreness in muscles
- Dry cough
- Headache
- Extreme level of lethargy
- High fever that may go over 100.4°F
How contagious can pneumonia be?
Bacterial strains like Streptococcus pneumoniae are often less contagious than the other forms. However, that does not mean you can totally eradicate the chance of pneumonia transmitting via bacterial strains. Always remember, there is not a single strain of bacteria or virus that is non-infectious in nature.
Presence of bacteria in your respiratory tract like throat or nose is quite normal, but there is a trick. If your immune levels are weak, the probability of you getting affected increases like crazy! Foreign Streptococcus pneumoniae can anytime attack your lungs and fill up the alveoli with fluid.
One of the most transmissible forms of bacteria responsible for causing pneumonia is Mycoplasma pneumoniae. If you even breathe in droplets of sneezes from an infected person with Mycoplasma pneumoniae, it can be extremely dangerous.
The spreadable period usually varies between 1-2 days, or may extend to several weeks depending on the infection type. You cannot specifically determine the time of exposure and incubation in children and adults, due to various underlying factors.
If you have taken antibiotics in the first 24 to 48 hours, then the chances of transmission automatically lowers. However, this time span may also differ from species to species. Treatment at the right time can save you from various life-threatening adverse effects of severe contagions.
When your pneumonia is a viral invasion, you are less likely to spread the disease post improvement from possible symptoms. Certain viral pneumonia can prove to be less transmissible in a day or two without a fever. Nevertheless, you may shed infectious viral substances enough to revive the disease in a healthy individual in the long term.
Which microbes cause pneumonia?
Bacterial species
Apart from Streptococcus pneumoniae, other bacterial strains are capable of causing pneumonia like-
- Legionella pneumophila: responsible for causing Legionnaire’s disease, which is a type of pneumonia (atypical).
- Mycoplasma pneumoniae and Chlamydophila pneumoniae also cause atypical pneumonia.
- Haemophilus influenza can result in both pneumonia and influenza. Adults with an age greater than 65 years have a high chance of getting pneumonia from influenza.
Viral species
You will mostly come across pneumonia in your adult stage because of the influenza virus. There are several viruses resulting in pneumonia in both adults and children, such as-
- RSV or respiratory syncytial virus, chickenpox (varicella) virus and measles virus. Influenza viruses and respiratory syncytial virus can lead to serious health complications in patients with pneumonia.
- Coronaviruses can cause severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) alongside lethal pneumonia.
Fungal species
Pneumonia resulting from fungi infections is less common than viral and bacterial ones. However, certain fungi species are still capable of triggering pneumonia like Coccidioides, Cryptococcus and Histoplasma.
You mostly come across fungal pneumonia if you have a not-so-strong immune system due to immunosuppressive disorders like HIV-AIDS. Your level of pneumonia probability from fungus also increases if you are under any medications that have altered effects on your immunity.
Studies have revealed that another fungal species going by the name of Pneumocystis carinii or Pneumocystis jirovecii can cause pneumonia. However, the possibility of pneumonia from P. jirovecii is quite low as compared to other microorganisms.
What are the diagnostic tests for pneumonia?
If you experience any of the probable symptoms of pneumococcal pneumonia, do not think twice before visiting a doctor. The diagnosis of any forms of pneumonia always begins with your medical history, which will reveal the following factors-
- Any person in the family who carries the contaminant
- Recent direct contact with an infected person (including exposure to sputum or respiratory droplets from sneezes or cough)
- Medications that you have taken in the past or currently taking that has an effect on your immune levels
After the doctor has jotted down your medical history, the process will follow a physical examination of possible symptoms. If more than one symptom indicated the possibility of pneumonia, the doctor will immediately go forward with some imaging tests.
Initially, your doctor will examine the sound of your lungs via breathing tests with a stethoscope. Your lungs will have fluid in the air sacs, which will cause a hindrance in the sound production. When you have acute pneumonia, the sound of your lungs will gradually diminish. There will be indicative crackling vibrations in certain areas due to coughing and wheezing.
Imaging tests common for pneumonia diagnosis
- X-rays of your chest to highlight whether there is the presence of pneumococcal strains. It is just a basic imaging test done to see the presence of the infection, not to identify the microbe. In other words, you cannot know the source of pneumonia (fungi, virus or bacteria) but can certainly confirm its presence.
- If certain cases of pneumonia, the doctor might go for a quick CT scan. It gives a more detailed result than X-ray, but again does not disclose the identity of the pathogen.
- There is a technique called pulse oximetry that helps in measuring the quantity of oxygen flowing in your bloodstream. Doctors use pulse oximetry to detect any decline in the level of oxygen content in your blood due to pneumonia. The process involves attaching a sensor to your ear or finger without causing any pain.
How to identify the nature of the causative microbe?
Bronchoscopy is a technique to visualize the insides of your respiratory tract, in search of infectious microbes. The process includes insertion of a long, thin tube into your trachea and vital bronchial airways. Whenever there is a need, the tube will take tissue specimens from the airways.
Doctors perform bronchoscopy mostly for severe cases of pneumonia in the elderly population. It can also come handy examination for patients who have shown deterioration in results, even after treatment with antibiotics.
Microbiological exams are the ones that actually help in identifying the pathogen behind the infection. Tests involve using your body fluids like blood or sputum for identification and characterization of the causative microbe.
To identify the presence of Legionella pneumophila and Streptococcus pneumoniae, doctors go for your urine sample. Apart from identification, microbiological tests can help in determining the specific antibiotic that can effectively work against the identified pathogen.
Remember that antibiotics can only treat pneumonia when the source is bacteria or fungi. There is no antibiotic treatment for viral pneumonia.