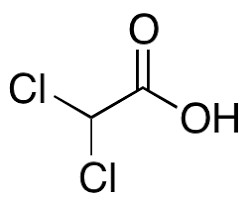
Often known as bichloroacetic acid, dichloroacetic acid is a fascinating compound with the scientific code CHCl2 (BCA). Think of it as a cousin to acetic acid, only it’s wearing a different outfit; two of the hydrogen atoms from the methyl group have been replaced by chlorine atoms.
The family of dichloroacetic acid is large, with many relatives in the form of salts and esters, each boasting a unique potential. Lately, the scientific community has been buzzing with excitement over the possibility of harnessing dichloroacetic acid for medical purposes. This is thanks to its talent for putting a brake on an enzyme called pyruvate dehydrogenase kinase.
Lab tests on animals and petri dishes suggest that dichloroacetic acid might slow down the progress of certain cancers. However, we’re still gathering puzzle pieces before we can confidently recommend it for cancer treatment.
Picture a world divided into northern and southern hemispheres, where unpredictability is the only predictable thing. That’s the world of dichloroacetic acid.
Belonging to the halogenated organic acids club, dichloroacetic acid transforms into the dichloroacetate ion when mixed with water. It possesses a potent pKa of 1.35, and it’s not to be taken lightly as it can cause harm if inhaled, potentially disturbing the mucus-lined hallways of our respiratory tract.
Interestingly, traces of dichloroacetic acid (DCA) can be found in the Asparagopsis taxiformis seaweed. We also see DCA appearing in chlorinated drinking water and as a side-product when our bodies break down chlorine-based drugs and substances. We can conjure up DCA by reducing its cousin, trichloroacetic acid. Alternatively, mix chloral hydrate with calcium carbonate, sodium cyanide, and water, followed by a dash of hydrochloric acid, and voila – you have DCA! Even the blend of hypochlorous acid with acetylene can lead us to DCA.
In the world of lab science, DCA and TCA play a significant role as agents that transition large molecules like proteins from liquid to solid.
Demonstrating their versatility, DCA and TCA have been used for both medical and cosmetic procedures. This includes the local vaporization treatment of genital warts and aesthetic applications such as chemical peels and tattoo removal. Intriguingly, these compounds can even be directed to annihilate healthy cells.
However, it’s not all smooth sailing. Although DCA sailed through safety checks in a randomized study, it didn’t quite hit the mark for newborns suffering from congenital lactic acidosis. A trial involving 15 children with MELAS, a condition that reduces mitochondrial activity and results in lactic acidosis, had to be halted prematurely. DCA’s neurological damage outweighed any discernible benefits.
The narrative for adult cancer patients isn’t much brighter. While DCA succeeded in reducing blood lactic acid levels, it didn’t improve the quality of life or extend survival times.
Therefore, despite early lab results hinting at potential benefits for lactic acidosis, comparative tests concluded that DCA’s impact was negligible. Moreover, drug toxicity reached a level where it was unsafe for patients to continue in trials.
In a promising turn, in 2007, a team led by Evangelos Michelakis from the University of Alberta revealed exciting results. Sodium dichloroacetate, a sodium variant of dichloroacetic acid, shrank tumors in rats and eradicated cancer cells in lab tests. Subsequently, a New Scientist article catapulted this simple, seemingly safe therapeutic approach into the limelight, hailing it as a potential cure for various types of cancer.
The accompanying commentary to the study lamented that without patent protection, pharmaceutical companies lack motivation to champion DCA as a cancer treatment. Subsequent discussions in the journal delved into potential side effects, including nerve damage. In the U.S., it’s worth noting that selling substances touted as cancer cures without FDA approval is strictly forbidden.
In 2012, the American Cancer Society cautioned that evidence supporting DCA as a cancer treatment was insufficient. Medical professionals agree: proceed with caution when it comes to DCA, and it should only be used within the confines of a controlled clinical trial.
Getting hold of this chemical may pose challenges. In a stark reminder of the dangers of deception, a scammer was sentenced to 33 months in prison for tricking cancer patients into buying ordinary starch, falsely claiming it was DCA.
Despite the cautionary tales, a study involving a small group of people with glioblastoma did proceed with DCA, not to gauge its effectiveness, but to test if a specific dose could be administered without harmful side effects like neuropathy.
The five study participants were concurrently undergoing other treatments. Experiments in labs and on animals suggest that DCA might be a hero in the fight against glioblastoma, triggering their dysfunctional mitochondria to self-destruct. Lab tests with neuroblastomas, characterized by flawed mitochondrial structure, showed DCA’s potential to combat these undying, cancerous cells.
Fast forward to 2016, a case report explored the potential of DCA in treating cancers affecting the central nervous system. Two years later, a study revealed DCA’s ability to make tumor cells change their metabolism from glycolysis to mitochondrial OXPHOS (the Warburg effect), enhancing oxidative stress levels. This heightened response was not observed in normal cells.
Neuropathy, a nerve-related complication, led to the premature end of several DCA clinical trials. However, an intriguing 2008 article in the British Journal of Clinical Pharmacology reported no such issues in other DCA cancer cure trials. The exact method by which DCA induces neuropathy remains a medical mystery.
Insights into DCA’s potential to cause neuropathic side effects emerged from studies conducted on lab-cultured neurons. These investigations revealed that DCA could strip away the protective layer around nerve cells over time and with dose intensity, a process known as demyelination. This condition appeared somewhat reversible once the drug was discontinued. Yet, a 2008 analysis of the same data suggested the nerve damage resembled a condition affecting sensory neuron axons rather than demyelination, citing a 2006 study by Kaufman et al.
Intriguingly, researchers are exploring the potential of DCA as a remedy for chronic heart failure resulting from blood vessel blockages. An added advantage of DCA is its ability to turbocharge metabolism by increasing NADH levels. However, if there’s sufficient oxygen available, NADH could be depleted. For more information, visit https://www.dcaguide.org/.